
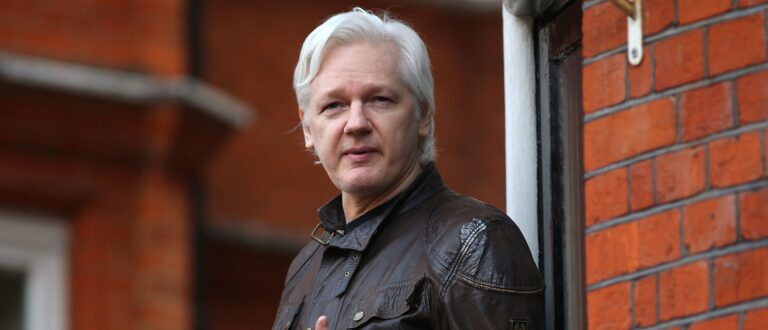
(Photography by Wade Hudson)
When it comes to diabetes drugs, there’s just something about Toronto researchers. In 1984, 63 years after Banting and Best isolated insulin, Daniel Drucker, another U of T alumnus, co-discovered glucagon-like peptide-1, or GLP-1, a gut hormone that lowers blood sugar and suppresses appetite. Drucker and Co.’s eureka moment was exciting-ish in endocrinology circles. But it wasn’t until decades later, when a GLP-1-mimicking drug called semaglutide proved effective for weight loss, that their work became the shot taken ’round the world.
SIGN UP TO READ THE BEST OF MACLEAN’S:
Get our top stories sent directly to your inbox twice a week
The ripples of the “Ozempic effect” are now unfathomably huge: a suite of ever-more GLP-1 drugs (Wegovy, Mounjaro and Rybelsus), a soon-to-be $100-billion industry, so many op-eds about our screwed-up body politics, witch hunts around celebrity users and, on a more serious note, widespread shortages that are expected to last through 2024. For Drucker, now a senior scientist at Toronto’s Lunenfeld-Tanenbaum Research Institute and a Canadian Medical Hall of Famer, Ozempic (and other GLP-1 drugs) is no vanity project. He’s already back in the lab.
You recently shot to fame as one of the pioneers of Ozempic, but you’ve been an endocrinologist for the last 40 years. What about diabetes initially piqued your interest? Or was it plain old scientific curiosity?
My first love was actually thyroid disease, thanks largely to my mentor, a specialist who came to U of T from Yale. In 1984, I went to Boston to work on a thyroid project at Massachusetts General Hospital. When I got there, they said, “That’s full now. You’ll have to work on this new glucagon thing.” I think I went home and said to my wife, “This seems like a loser project, but I’m just gonna make the best of it.” And, well, we know what happened.
You and some of your international colleagues discovered the diabetes-fighting potential of insulin’s cousin, GLP-1, which eventually led to the creation of Ozempic. Did you have any inkling back then of the magnitude of what you’d stumbled on?
I was excited by the results, but I was equally excited by the fact that my boss was excited about them. I was a 28-year-old trainee making $20,000-something a year. I had a child—and a lot more black hair than I do now—but not a lot of job security. I thought, This is cool, but another part of my brain was thinking, Maybe I can publish some papers. Maybe I’ll get a job.
Later on, your research involved a venomous lizard—a Gila monster, to be precise. Whose idea was that?
The person who deserves credit for that is John Eng, an endocrinologist from the Bronx. He sequenced proteins from the lizard’s venom and found two that looked like human GLP-1: exendin-3 and 4. I read his papers in 1992 and said, “That’s really weird! Does the lizard have GLP-1, too?” To answer that, I had to clone its genes.
How did you do that?
First, I tried to get some DNA from dead lizard chunks stored at the Royal Ontario Museum. The ROM’s lizard specialist, Bob Murphy—who’s still there—had some in the freezer. When that didn’t work, we had to get a live Gila, which aren’t sold in the pet stores at the mall. The most reputable person who could get me one was a guy who ran the Utah Zoo. He just said, “250 bucks.” Murphy arranged all the permits.
Can you gauge for me the level of excitement around GLP-1 way back when?
When I gave talks about it at the Endocrine Society in the ’90s, there was usually one person in the room. There were already pills you could take to stimulate insulin secretion, so people were like, “Why would you inject something that comes from a poisonous lizard?” It took a long time for enthusiasm to build.
Flash forward 30 years and things couldn’t be more different: Ozempic is advertised everywhere. Rybelsus has its own billboard up the street from my house. Do you ever feel bitter about the fact that it took these meds becoming weight-loss remedies for people to get excited about your work?
No. In science, you have a one in 10,000 chance of your research going from lab to drug. I’ve been involved with the GLP-1 discovery, and also drugs like Januvia (for Type 2 diabetes) and Gattex (for short bowel syndrome). It’s an unbelievable privilege to be associated with science that treats human disease, and I’ve won the lottery over and over again. Bitter is the last word that would cross my mind.
Pharma companies have always been in the business of “miracle drugs,” but GLP-1 might be the one class of meds in recent memory that seems to warrant its hype. Yes, they’re normalizing people’s blood sugar levels, but they also quiet the constant mental hum of food cravings. Patients who have struggled with obesity their entire lives are finally losing weight. For the skeptics out there: are these drugs too good to be true?
So, there’s no free lunch, so to speak. Gastrointestinal complaints are the most common side effects, but half of people don’t have them. The reports we’re seeing of bowel obstructions are rare. These drugs aren’t a panacea, but the risk-benefit ratio is generally very positive. What does worry me is people shipping themselves some 1-800 mail-order, black-market drugs without first talking to a doctor.
Some experts have said that we may also look back on GLP-1 drugs as one of the greatest modern advancements in the treatment of chronic conditions. They’ve already shown promise for cardiovascular, liver and kidney disease, and some are now being tested on Alzheimer’s, sleep apnea, PCOS—even addictive behaviours, like gambling. That is a huge scope.
Are these drugs going to help all of these different conditions in a meaningful way? That’s unlikely. We don’t yet have enough data to say we should put this stuff in the drinking water, but there are encouraging signs of their benefits. Right now, we have excellent data for Type 2 diabetes, heart disease and obesity. We’re gonna get some excellent data for kidney disease in the next few months, then heart failure in the summer. We’ll have to wait a year or two for Parkinson’s and Alzheimer’s.
A future with less chronic disease? There’s a rare bit of good news for the Canadian health-care system!
Maybe. Again, we can’t assume anything until we have the data. Health-care economists already study this sort of thing, though: how much do the drugs cost? How many people will we have to treat to see a major expense reduction? Let’s wait to see stats. Sorry, I’m so boring.
Food-industry experts seem to think Ozempic is starting to change our shopping habits. The CEO of Novo Nordisk, the Danish manufacturer of Ozempic and Wegovy, has apparently already been fielding worried calls from junk-food suppliers.
Less than one per cent of people with obesity are taking these drugs, so I think a lot of that is hype, too. When some businesses miss their targets, they go, “It was the Ozempic effect!” It’s a convenient excuse. Walmart just claimed that shoppers who use Ozempic and Wegovy are buying less food.
Ozempic’s certainly provided an interesting Rorschach test for our cultural neuroses around weight. There’s hope that the rise of GLP-1 drugs might help pry us away from the mindset that obesity is a moral failing, rather than a complex biological process. Have you had those chats with your peers?
Yes, and that “moral failing” bias extends to health-care professionals, too. For decades, I’ve had patients do everything I ask them to—limit non-healthy foods, exercise to the maximum extent they can—and they still struggle to lose weight. Drugs like Ozempic have allowed them to say, “See? I needed help, just as I would with Crohn’s disease or MS or any one of 150 other diseases a person can’t just will away.”
Witnessing those before-and-afters must be pretty powerful.
It’s hard for me to go out and not meet someone who’s taken these drugs. Recently, a close family member came up to me at a party and said, “It used to take me an hour to go food shopping, because I’d have to read every label and see how many calories and what percentage of fat was in each product. I had to scrutinize everything I put in my cart. Now, it takes me 15 minutes. I’m not going to overeat and I’m healthier.” Wow, you know?
There’s also the flip side, though: “Taking Ozempic? You’ve taken the easy way out. Don’t bother calling yourself body positive.” What do you make of that backlash?
Someone recently sent me an article about body-positive influencers—some with a lot of followers—who are going from espousing the view that we should be comfortable with our size to accepting money from drug companies to say, “Hey, what about Ozempic?” I understand the backlash to that. I also know that, on social media, people take pleasure in taking shots at other people without having lived in their bodies.
You’ve provided guidance to Novo Nordisk on GLP-1 drug development. What recommendations did you give them?
One is to avoid supply-chain issues. These companies have admitted they didn’t anticipate the phenomenal demand for their blockbuster drugs. It’s going to take time—and billions of dollars—to build more plants, which they’re doing now.
To help stem the Ozempic shortages, the Ontario government recently changed its listing under the provincial drug benefit program. Now, people who use Ozempic off-label—for weight loss rather than diabetes—will have to pay out-of-pocket. In Canada, that amounts to roughly $300 a month. Do you think that was a wise move?
When you have a shortage, you have to prioritize the people at the greatest risk. But pharmacists don’t ask patients, “Do you really need this drug?” It’s a challenging discussion, but decisions have to be made. Whether or not this is just a convenient way for the government to limit supply, you’d have to ask them.
What else have you told Novo Nordisk?
There’s no point in having an amazing, helpful drug if people can’t afford it. We’ve had such ethical conversations before—with HIV, hepatitis, COVID vaccines. The story of insulin hasn’t been a great look for the States. Until very recently, it was still prohibitively expensive—and people were still dying—100 years after its discovery. That shouldn’t happen in wealthy societies.
Your name is also listed in Novo Nordisk’s literature about the discovery of Ozempic. I know you’re not in the research biz for the money, but do you receive royalties?
The GLP-1 drugs brought in some revenue to Mass General—and my boss—but not me. I’ve never received a loonie.
Damn.
I don’t know what I’d do with that money, to be honest—maybe my grandchildren would never work? I have a good life, but I don’t drive fancy cars or wear expensive clothes. My wife’s always saying, “Why don’t you buy a new suit?” I have six suits!
Have you seen Oppenheimer?
I have.
Do you have any Pandora’s box–style worries about Ozempic and its ilk? Any regrets about what you’ve helped unleash?
Ten years ago, I would’ve been more anxious. Around 2011, there were concerns that GLP-1 drugs could cause pancreatitis and cancer. Public Citizen, an entity that scrutinizes drug safety, petitioned the FDA to remove them from the market. We didn’t have the data we have now—or the benefit of seeing millions of people successfully treated over the course of 19 years. So I don’t lie awake at night, but I respect what I don’t know. I’ll never say these drugs are completely safe, or that we’ll never learn anything more about them. That’s just not me—and that’s not how medicine works.
It occurs to me that someone who’s chosen to work in a lab for a living might not be suited to the level of attention that Ozempic has generated. Has that spotlight changed the way you work?
I’m turning down a lot more invitations to speak due to time constraints. That’s a nice problem to have. Our lab feels really good about the work, but it doesn’t change the science we do. I’d rather look at a cool picture my granddaughter drew than review the latest sales of Mounjaro.
Is there such a thing as a sophomore slump for scientists? How do you follow Ozempic?
In January, our team published a brand-new finding in Cell Metabolism that showed that GLP-1 reduces inflammation in the body’s peripheral tissues, like the lung and white blood cells, through the brain. A lot of what GLP-1 does is magic, and we’re still trying to figure out how the magic happens. We’re 40 years into this story, but we could just be at the beginning.
#Canadian #doctor #helped #invent #Ozempic



















+ There are no comments
Add yours